

CONSULTANT:: | DR MOHIT ARORA |
SPECIALITY:: | M.D. AY. MEDICINE, DIP CRITICAL CARE MEDICINE |
Dr. Mohit Arora has completed his graduation (B.A.M.S) in the year 2009 from Rajiv Gandhi University of Health Sciences. He completed his M.D. in Ayurvedic Medicine in the year 2014 from Rajiv Gandhi University of Health Sciences. He joined as a Asst. Professor in Ayurvedic medical college in the year 2014. He teached students there for six months and then started serving in govt. of Haryana. He has also worked in intensive care unit and cath lab to learn various life saving procedures and to treat critical patients. He has completed his P.G.Diploma in critical care medicine in the year 2020.
Dr. Mohit Arora has a view of treating the patients in Ayurveda and Allopathy system of medicine to give them complete care and intensive treatment. He has done his dual specilaization.
Vitiligo is a condition in which the skin loses its pigment cells called as melanocytes. This can result in discolored patches in different areas of the body, including the skin, hair and mucous membranes.

Psoriasis is a skin disease that causes red, itchy scaly patches, most commonly on the knees, elbows, trunk and scalp. Psoriasis is a chronic inflammatory disease that really affects the life of a person.
The common clinical features are:
There are several types of psoriasis, including:
Plaque psoriasis. The most common form, plaque psoriasis causes dry, raised, red skin patches (lesions) covered with silvery scales. The plaques might be itchy or tender, and there may be few or many. They usually appear on elbows, knees, lower back and scalp.
Nail psoriasis. Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth and discoloration. Psoriatic nails might loosen and separate from the nail bed called as onycholysis
Guttate psoriasis. This type primarily affects young adults and children. It's usually triggered by a bacterial infections. It is marked by small, drop-shaped, scaling lesions on the trunk, arms or legs.
Pustular psoriasis. This rare form of psoriasis causes clearly defined pus-filled lesions that occur in widespread patches (generalized pustular psoriasis) or in smaller areas on the palms of the hands or the soles of the feet.
Erythrodermic psoriasis. The least common type of psoriasis, erythrodermic psoriasis can cover your entire body with a red, peeling rash that can itch or burn intensely.
Psoriatic arthritis. Psoriatic arthritis causes swollen, painful joints that ar

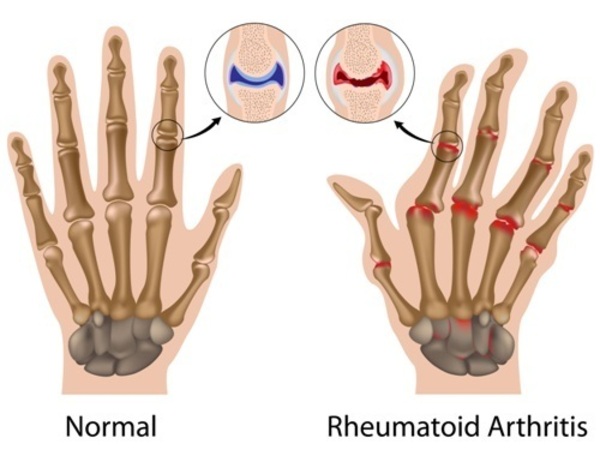
Rheumatoid arthritis (RA) is an autoimmune disease that can cause joint pain and damage throughout your body. The joint damage that RA causes usually happens on both sides of the body. In rheumatoid arthritis, the body's immune system attacks its own tissue, including joints. In severe cases, it attacks internal organs also.
SYMPTOMS:
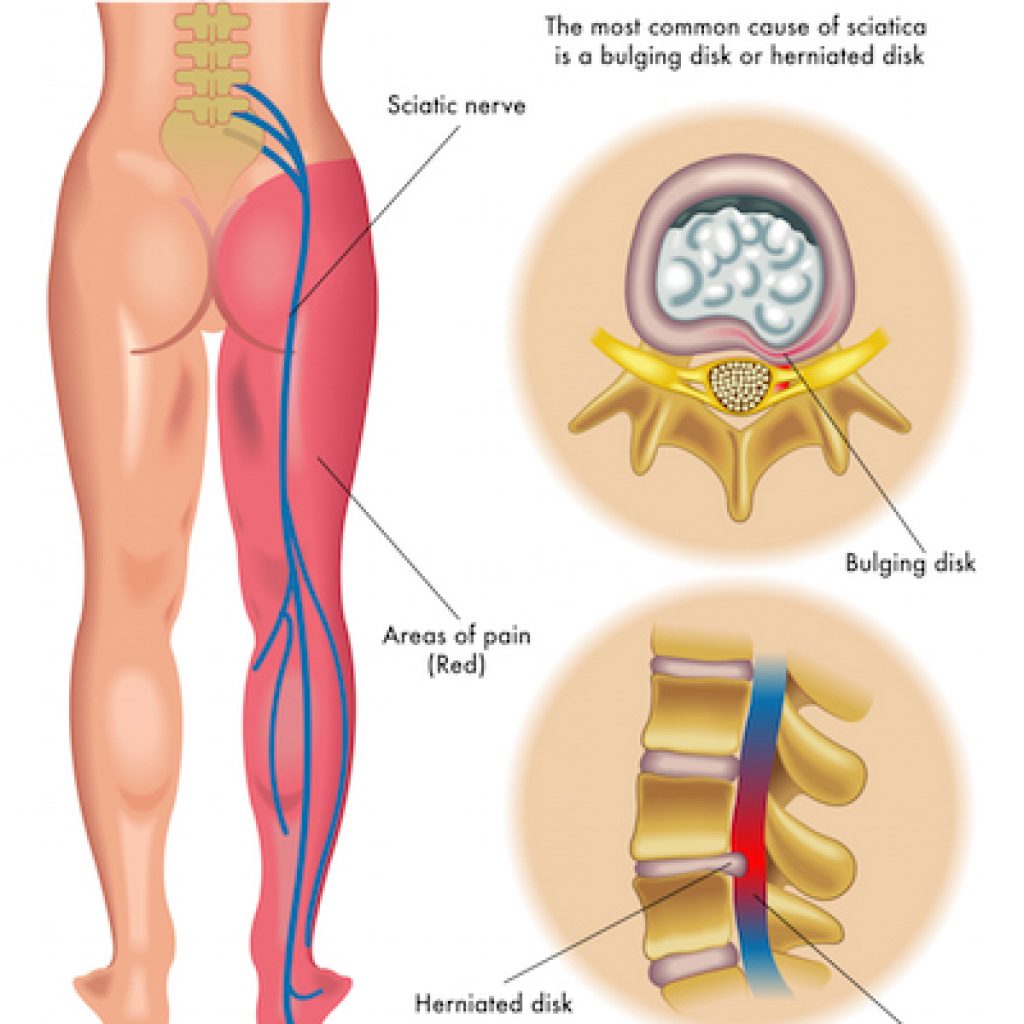
The low back supports the weight of the upper body and provides mobility for everyday motions such as bending and twisting. Muscles in the low back are responsible for flexing and rotating the hips while walking, as well as supporting the spinal column. Nerves in the low back supply sensation and power the muscles in the pelvis, legs, and feet.
Most acute low back pain results from injury to the muscles, ligaments, joints, or due to discs problems.
Cause:
As you age, the bones and cartilage that make up your backbone and neck gradually develop wear and tear. These changes can include:
Depending on the underlying cause of the pain, symptoms can be experienced in a variety of ways i.e.
a) Pain that is dull or achy contained to the low back.
b) Stinging, burning pain that moves from the low back to the backs of the thighs, sometimes into the lower legs or feet; can include numbness or Muscle spasms and tightness in the low back, pelvis, and hips.
c) Pain that worsens after prolonged sitting or standing.
d) Difficulty standing up straight, walking, or going from standing
The two common types to categorize the back pain includes:
There can be a traumatic pain as well.
In addition, symptoms of lower back pain are usually described by type of onset and duration:
Acute pain. This type of pain typically comes on suddenly and lasts for a few days or weeks, and is considered a normal response of the body to injury or tissue damage. The pain gradually subsides as the body heals.
Subacute low back pain. Lasting between 6 weeks and 3 months, this type of pain is usually mechanical in nature (such as a muscle strain or joint pain) but is prolonged. At this point, a medical workup may be considered, and is advisable if the pain is severe and limits one’s ability to participate in activities of daily living, sleeping, and working.
Chronic back pain. Usually defined as lower back pain that lasts over 3 months, this type of pain is usually severe, does not respond to initial treatments, and requires a thorough medical workup to determine the exact source of the pain.
Symptoms:
Cervical spondylosis is also called cervical osteoarthritis. It is a condition involving changes to the bones, discs, and joints of the neck. These changes are caused by the normal wear-and-tear of aging. With age, the discs of the cervical spine gradually break down, lose fluid, and become stiffer. Cervical spondylosis usually occurs in middle-aged and elderly people. As a result of the degeneration of discs and other cartilage, spurs or abnormal growths called osteophytes may form on the bones in the neck. These abnormal growths can cause narrowing of the interior of the spinal column or in the openings where spinal nerves exit, a related condition called cervical spinal stenosis.
Causes:
The bones and protective cartilage in your neck are prone to wear and tear that can lead to cervical spondylosis. Possible causes includes:
Symptoms:

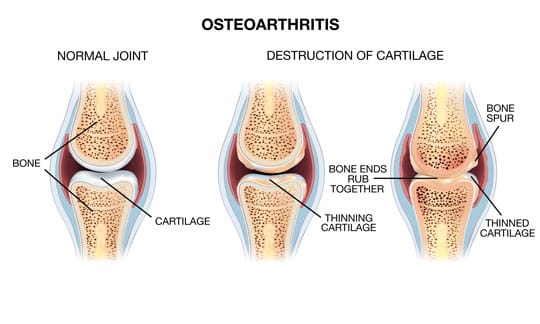
Osteoarthritis is a degenerative disease and most common type of arthritis. It is characterized by focal loss of articular hyaline cartilage with formation and remodeling of a joint. Cartilage provides a smooth surface to allow free movement of joint, provides a cushioning, and for joint stability. Cartilage can become frayed, cracked, and degenerates. Eventually it can worsen and effectively the cartilage fails and then ends of the bones rub and bang on each other. Bones have nerves and this is when the joints become painful. Osteoarthritis can occur without a history of joint injury. However an injury to the joint ligaments, and/or injury to the joint cartilage can lead to osteoarthritis at a later time. This is called post traumatic osteoarthritis.
Symptoms:
One of the risk factors for osteoarthritis that we do have control over is body weight. Excess body weight has direct effect on osteoarthritis. Individuals who are overweight (Body Mass Index of 25 to 29) are 2.5 times more likely to develop knee osteoarthritis and those who were obese (body mass index of >30) are 4.6 times more likely to develop osteoarthritis.
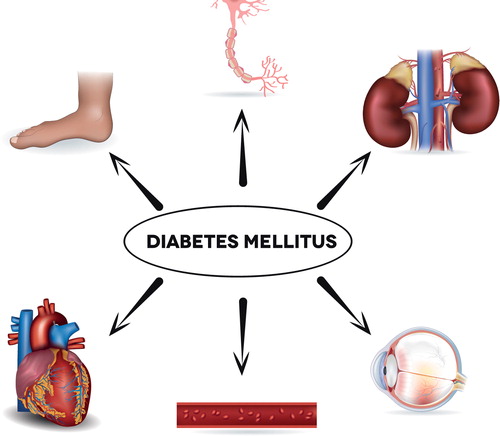
Diabetes mellitus (DM), commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased appetite, tiredness, fatique, pruritus, nausea, vomiting, mood changes .
Types:
Type 1 diabetes: This type is an autoimmune disease, meaning your body attacks itself. In this case, the insulin-producing cells in your pancreas are destroyed so the production of insulin in the body is very less or the production of insulin is completely stopped.It is also called insulin-dependent diabetes.
Type 2 diabetes: With this type, your body either doesn’t make enough insulin or your body’s cells don’t respond normally to the insulin.
Prediabetes: This type is the stage before type 2 diabetes. Your blood glucose levels are higher than normal but not high enough to be officially diagnosed with type 2 diabetes.
Gestational diabetes: This type develops in some women during their pregnancy. Gestational diabetes usually goes away after pregnancy, however, if you have gestational diabetes you're at higher risk of developing type 2 diabetes later on in life.
Causes:
Complications of Diabetes Mellitus:
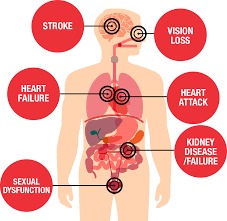
It is a silent killer affecting your brain, heart, kidneys, nerves involving multi organ system.
Hypertension is another name for high blood pressure. It can lead to severe health complications and increase the risk of heart disease, stroke, and sometimes death. Blood pressure is the force that a person's blood exerts against the walls of their blood vessels.
When there is no specific underlying cause for hypertension, it is called as essential hypertension.
Causes:
Health care tips to avoid hypertension:
People should exercise on at least 5 days of the week like walking, jogging, cycling, or swimming.
Stress reduction can help a person to control blood pressure.
Avoid eating fast food.
Control your cholesterol & triglyceride levels.
Hypertension if uncontrolled can lead to multiorgan system involvement.
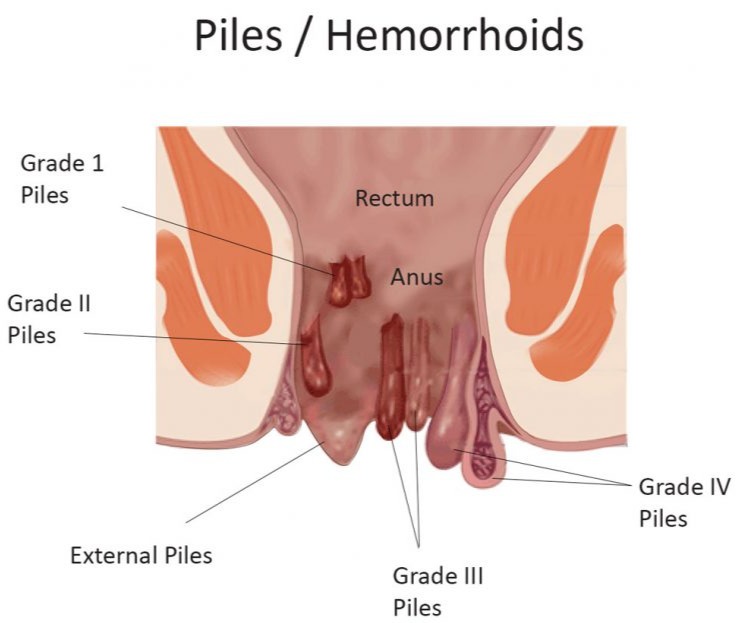
Piles are swollen and inflamed veins in the rectum and anus that cause discomfort and bleeding. The size of piles can vary, and they are found inside or outside the anus. Piles occur due to chronic constipation, chronic diarrhea, lifting heavy weights, pregnancy, or straining when passing a stool.
Hair loss (alopecia) can affect just your scalp or your entire body, and it can be temporary or permanent.
It can be the result of heredity, hormonal changes, medical conditions or a normal part of aging. Anyone can lose hair on their head, but it's more common in men.
Baldness typically refers to excessive hair loss from your scalp. Hereditary hair loss with age is the most common cause of baldness.
Signs and symptoms of hair loss may include:

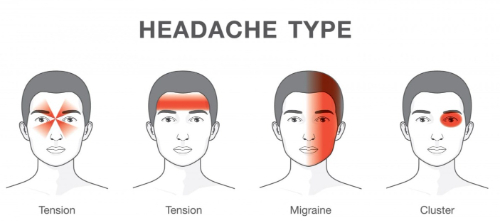
A migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It's often accompanied by nausea, vomiting, and extreme sensitivity to light and sound.
Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.
Migraine headaches are sometimes preceded by warning symptoms. Triggers include hormonal changes, certain food and drink, stress and exercise.
Prodrome
Hours or days before a headache, about 60% of people who have migraines notice symptoms like:
Aura:
These symptoms stem from your nervous system and often involve your vision. They usually start gradually, over a 5- to 20-minute period, and last less than an hour. Patients may experience:
Irritable bowel syndrome (IBS) is characterised by recurrent abdominal pain in association with abnormal defecation in the absence of a structural abnormality of the gut. Young women are affected 2–3 times more often than men. Coexisting conditions, such as non-ulcer dyspepsia, chronic fatigue syndrome, dysmenorrhoea and fibromyalgia, are common.
Common signs & symptoms:
Psychological disorders such as anxiety and depression are also likely to occur to individuals, often due to the discomfort or embarrassment that arises because of IBS.
Common Causes:
Some of the common causes of IBS include:

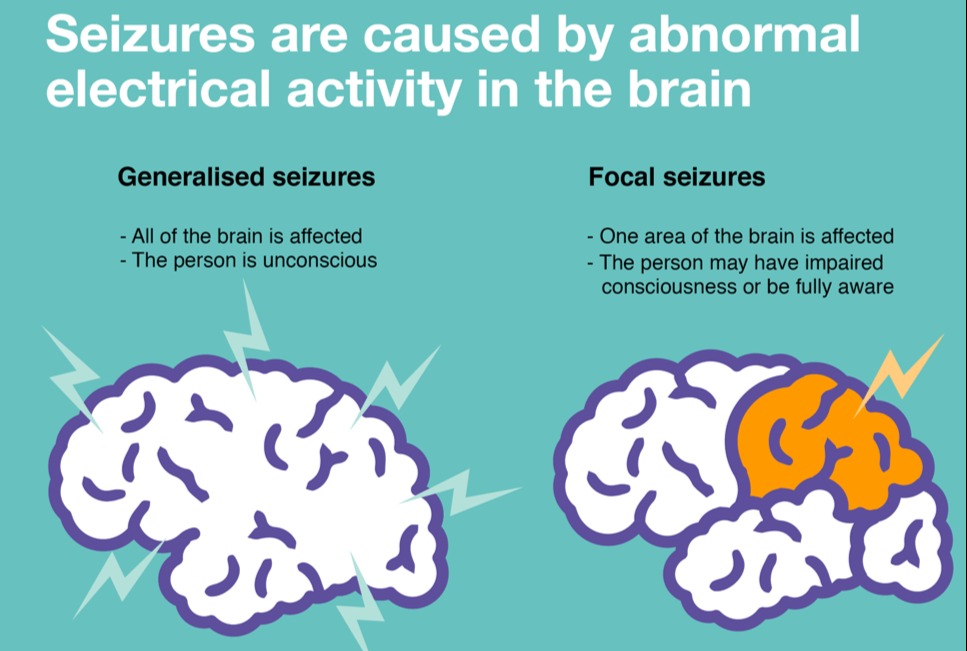
Epilepsy is a neurological disorder in which brain activity becomes abnormal, causing seizures or periods of unusual behavior, sensations, and sometimes loss of awareness.
Epilepsy may occur as a result of a genetic disorder or an acquired brain injury, such as a trauma or stroke.
Seizure types are divided into two major groups:
The Ayurvedic treatment for epilepsy has shown efficient results in decreasing the number of attacks & intensity of attacks. Also the time intervals between attacks has significantly increased.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF PSORIASIS.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF VITILIGO.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF HAIR FALL.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF OSTEOARTHITIS.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF RHEUMATIC ARTHRITIS.
HE HAS TREATED VARIOUS PATIENTS OF LUMBAR & CERVICAL SPONDYLOSIS.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF LUMBOSACRAL SPONDYLOSIS.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF IRRITABLE BOWEL SYMDROME.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF CHRONIC ALLERGIC COUGH AND ALLERGIC RHINITIS.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF PILES WITH MEDICINE ONLY.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF MIGRAINE.
HE HAS TREATED SUCCESSFULLY VARIOUS PATIENTS OF RENAL STONE.







